
Overall, there was a significant difference in pre- and postsedation ETCO 2 levels in all groups however, none of the children needed ventilatory assistance. Nearly half of all children who received combination drugs showed signs of respiratory depression with hypoxemia (54.5%) and hypercarbia (45.5%).

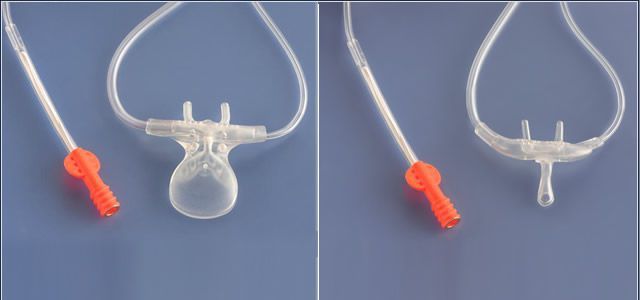
Hypercarbia was detected in about 30% ( n = 13) of the cases, and in 38% ( n = 5) of them, it was not accompanied by hypoxia. They were reported as three groups based on the drugs received: midazolam alone, ketamine alone, or midazolam in combination with ketamine or fentanyl. Forty-four children who did not have significant organ failures were monitored for respiratory depression by comparing pre- and postsedation ETCO 2 (hypercarbia defined as >10 mm Hg rise) and SpO 2 (hypoxemia defined as <92%). A simple nasal cannula interface with side-stream capnography could be useful in nonintubated patients if it provides a good correlation with partial pressure of carbon dioxide in arterial blood (paCO 2).Īslan et al., 3 in their simple yet informative study published in the current issue of the Indian Journal of Critical Care Medicine, have addressed this important aspect by examining the effects of sedation and analgesia on ETCO 2 measured by side-stream capnography in their PICU during the central venous catheter placement. 2 End-tidal carbon dioxide by mainstream as well as side-stream capnography is a standard of care during intubation and as a part of multiparameter monitoring in children on mechanical ventilation in PICU. The American Society of Anesthesiologists Task Force on moderate PSA recommends continuous monitoring and recording of the level of consciousness, ventilation, and oxygenation as well as hemodynamic parameters by an additional person responsible for patient monitoring. Abnormalities in ventilatory function and hypoventilation during PSA are detected earlier by end-tidal carbon dioxide (ETCO 2) monitoring than by pulse oximetry, as hypoxemia would be a late sign given the physiology of oxygenation and the practice of supplemental O 2 during PSA. Objective measurements by pulse oximetry oxygen saturation (SpO 2) are commonly performed in most centers.

1 Visual assessment of respiratory rate, depth, accessory muscle use, and chest auscultation are informative regarding patient's respiratory effort however, they are subjective.
Respiratory depression (4–5%) and the need for assisted ventilation (0.5–1%) during PSA have been reported especially when performed by nonanesthetists and outside the operation theater setting. Procedural sedation and analgesia (PSA) in children is challenging as it depends on cooperation from the child that varies with chronological age, behavioral, emotional, and cognitive development. Striking a balance between optimizing pain control and comfort during procedures and minimizing the risk of sedation-related complications are indispensable, more so in a spontaneously breathing patient. Procedural interventions are an integral part of monitoring and management in pediatric intensive care units (PICU).


 0 kommentar(er)
0 kommentar(er)
